Late Side Effects
Some early side-effects described above can persist for years, although their nature and impact will likely change over time. Other late side-effects may only develop after many years however. These often result from the damage caused to blood vessels during radiation treatment of the original cancer. Because blood vessels nourish nerves, muscles and bones, if nourishment is prevented, then these tissues gradually alter and even decay over time. It is always important to follow up any changes in your body with your doctor or oncologist, no matter how long after the original treatment, as late-side effects can themselves pose serious threats to your health and well being.
Dry mouth (xerostomia)
If you still experience xerostomia (or dry mouth) for more than two years, then the damage to your salivary glands are likely to be permanent. While early side-effects focussed on difficulties in eating and drinking, late side effects include long-term damage to your teeth through poor oral hygiene, which can lead to the onset of osteoradionecrosis - see below. Xerostomia may also lead to burning mouth syndrome, a burning sensation that can affect anywhere in the mouth including throat, tongues, gums, lips, palate.
If burning mouth syndrome occurs, temporary relief can be found through eating and drinking. For longer term solutions, avoidance of certain types of food and drink may be necessary (such as spicy food and alcohol), and taking tobacco. Like management for tinnitus, cognitive behaviour therapy might be suitable for some people.
Muscle and joint stiffness (Fibrosis)
Radiation-induced fibrosis usually occurs within months after treatment has finished, and can take many years to develop fully. Fibrosis is the excessive formation of fibrous connective tissue, a result of radiation damage to tissues, that can occur in muscles, skin, subcutaneous tissues, organs and even bones. It results in the stiffening over time of muscles and joints, and can lead to severe mobility issues. For head and neck cancer patients, this may result in stiff neck and shoulders, and trismus (the inability to open the jaw very wide). Fibrosis may also occur over time in the throat, making swallowing difficult, as those muscles become tighter.
While radiation-induced fibrosis cannot be stopped, its effects can be countered through doing daily exercises for life, such as stretching the neck muscles, rolling the head clockwise and anticlockwise, shoulder shrugs and rolls, and jaw stretching exercises to name but a few. A type of massage called myofascial release can also help. If fibrosis affects your ability to swallow, then see your doctor for a referral to a speech and language therapist.
Jaw pain and stiffness (Trismus)
Trismus is the inability to open the jaw fully to eat or drink. It is a side-effect of radiation damage to muscle fibres in the jaw, causing fibrosis (see above). As well as eating and drinking, chewing, oral care, and speech and language can be impacted as well.
Your speech and language therapists will provide you with simple exercise regimes to use during and after treatment to help reduce this side effect, e.g. jaw stretching exercises. It is recommended you do these as a prophylactic to reduce any future impact that trismus may have.
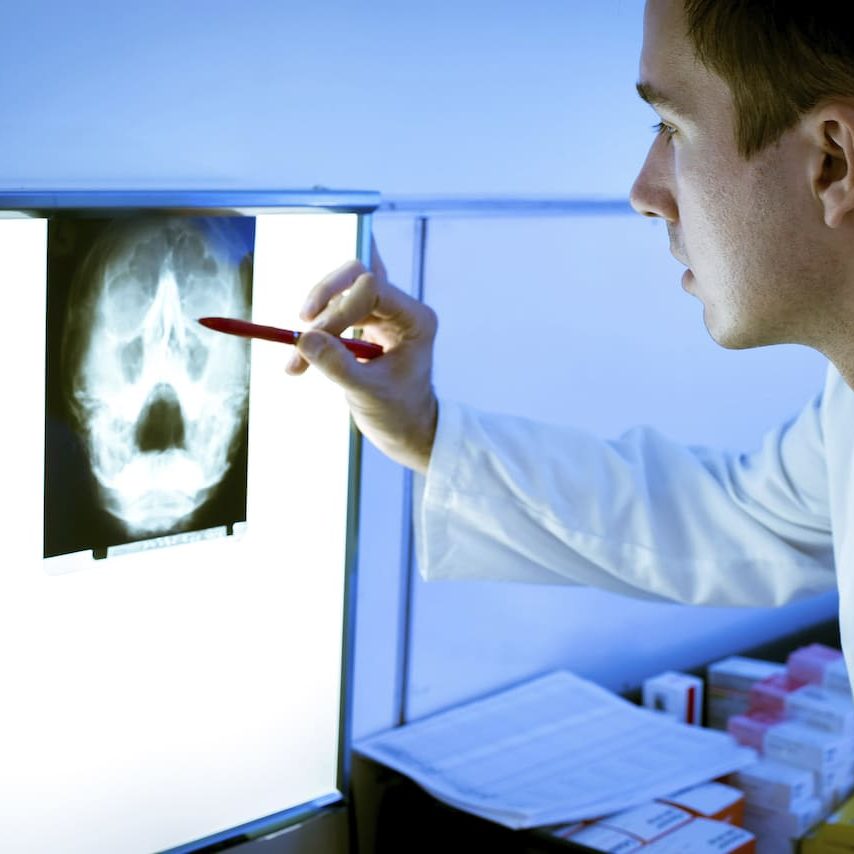
Osteoradionecrosis
Osteoradionecrosis is a complication of radiotherapy. This typically develops in the months or years following completion of radiotherapy. It is the necrosis (death) of jaw bone due to the body's impaired ability to heal and maintain tissues after irradiation. The condition affects 7-10% of people who have had radiotherapy and is more likely to occur if you:
- Have had dental extractions after radiotherapy
- Needed a large number of dental extractions before radiotherapy
- Smoked, especially during or after radiotherapy
- Have poor oral hygiene during or after radiotherapy
- Receive a high radiotherapy dose to the lower jaw bone
Prevention is the best management of osteoradionecrosis. A restorative dentistry assessment involving “prehabilitation” and dental extractions (if required) is crucial to reducing the risk for osteoradionecrosis. Please see the oral rehabilitation section for more information. Long-term recall (dental check-ups) is also important to maintaining your oral health and, therefore, preventing dental infections and the need for dental extractions, which may increase the chances of osteoradionecrosis.
If dental extractions are required, it is important to re-evaluate the dose of radiotherapy given to the patient to determine the risk of osteoradionecrosis. Dental extractions may be undertaken in stages and combined with other treatments such as antibiotics, mouthwashes, and certain medications. There is no clear evidence on the best way to prevent osteoradionecrosis if dental extractions are required.
Most cases of radiotherapy affect the lower jaw (approximately 90% of all cases), and can start with jaw pain or aching. In some cases, there may be no symptoms in the early stages of necrosis. Osteoradionecrosis is caused by a combination of changes to the strength of your jaw bone (which becomes more scarred/fibrous) and a reduced blood supply to the jaw bone. It is difficult to treat osteoradionecrosis, and there is not an effective cure for this.
In some cases, when the area of necrosis is very small, it may heal over time. Your doctor may prescribe antibiotics or a mouthwash to treat an infection and help you clean the area effectively.
It is common for loose fragments of bone to either be removed by a healthcare professional, or for these to come out by themselves. In some cases, the maxillofacial surgeon will clean the area surgically and remove larger areas of bone.
In addition, certain medications may help the tissues heal after osteoradionecrosis. There is no clear evidence whether any of these help; however, there is ongoing research in this area. One clinical trial (the RAPTOR trial) is investigating the use of three different medications in combination to treat osteoradionecrosis.
Osteoradionecrosis can progress, often at a slow rate. This can lead to infection coming out from the jaw bone or face. If left untreated, the condition can be life-threatening. In rare cases, the maxillofacial surgery team may remove a large portion of jaw bone in a similar manner to a cancer resection. They may then leave the remaining jaw bone to heal, using a plate to join separated fragments. Alternatively, the area may be reconstructed with a free flap, typically from your leg, hip, or shoulder. This surgery is difficult for the surgeon for the reasons outlined above: your tissues will be altered by radiotherapy and will, therefore, be more scarred and have less of a blood supply.
Note – “Free flap surgery” involves the transfer of a patient's own tissue from a donor site to a recipient site, which is typically the site of a defect. The donor site usually has a distant location with respect to the recipient site.
Fingers and toe numbness, pain and tingling (CIPN)
Chemotherapy Induced Peripheral Neuropathy (CIPN) is where hands and feet experience numbness, tingling (“pins and needles”) or pain. CIPN can last for weeks, months, or even years after treatment is done. If the condition worsens, these symptoms may start to spread further up the arms and legs. Parts of your face and neck may also feel numb to touch or movement as well. CIPN can be permanent if it hasn’t disappeared after 6-9 months.
The risk of CIPN depends on the type of chemotherapy and dose given, and increases with each cycle of chemotherapy. CIPN can make it hard to get around and do things you used to do.
CIPN can cause severe pain and can affect things like the way you walk, write, button your shirt, or pick up coins. If it gets worse, it can also cause changes in your heart rate and blood pressure, falls, trouble breathing, and not being able to move on your own. It’s important to let your cancer care team know if your symptoms get worse.
Try to exercise fingers by pressing the fingers on both hands together as a "steeple" to pressure the fingers together. Alternatively press each finger to your thumb a few times then repeat regularly through the day.
Try to wiggle your toes to improve circulation to them and rub your toes regularly to reduce the stiffening feeling.
Keep your hands and feel as warm as possible, Wear gloves and thick socks as cold will make the CIPN worse.
Thyroid issues (Hypothyroidism)
Radiation treatment to the head and neck can cause hypothyroidism in many patients, because the radiation damages the thyroid gland in the lower neck, affecting its ability to produce hormones critical in regulating the body’s growth and metabolism. Side effects include physical and mental sluggishness, leading to weight gain, fatigue, dry hair and skin, hair loss, constipation, memory decline and depression. The extent of effects on people are however very varied.
Ensure you have annual blood checks to check on both thyroid stimulating hormone (TSH) and thyroxine (a type of thyroid hormone also known as free T4) levels. If levels of these hormones are lower than normal then you may have hypothyroidism, and you may be prescribed a thyroid hormone replacement.
Dry Skin conditions (Xeroderma)
Itchy, dry or rough skin conditions akin to eczema can occur on head and neck areas, particularly where the skin was exposed to radiotherapy. This may be linked to pre-treatment allergies and skin conditions that have lain dormant for year but flare again post treatment.
- Moisturize. Moisturizer seals in water to help keep your skin's protective barrier healthy. Use moisturizer throughout the day, especially on the hands. And before going outdoors, use a moisturizer that contains sunblock or a broad-spectrum sunscreen with an SPF of at least 30, even on cloudy days. Apply sunscreen generously and reapply every two hours — or more often if you're swimming or sweating. Cetraben moisturiser for day time and ointment for sleeping is available without prescription at most chemists and is highly effective. This medication does not contain hydrocortisone steroid. If Cetraben does not relieve the itchiness and dry skin, then refer to your GP or Head and Neck nurse support team.
- Limit water exposure. Keep bath and shower time to 10 minutes or less. Use warm, not hot, water. Rinse and pat dry. Try to bathe no more than once a day.
- Use a gentle cleanser or allergen-free soap. Try a nonsoap cleansing cream or shower gel. Or use fragrance-free moisturizing soap with no alcohol or allergy-causing substances (hypoallergenic soap). Rinse thoroughly and pat dry. Apply a moisturizing cream while your skin is still damp.
- Shave with care. Shaving can be drying. If you shave, use a lubricating agent before you start. Shave in the direction of hair growth, unless that irritates your skin. Use a sharp blade and rinse it with warm water after each stroke. When done, apply moisturizer.
- Cover as much skin as possible in cold or windy weather. Harsh weather can be especially drying to skin. Scarves, hats, and gloves or mittens help protect your skin when you're outdoors.
- Rinse and moisturize after swimming. This is especially important if you've been swimming in a heavily chlorinated pool.
- Drink when you're thirsty. Drink noncaffeinated beverages each day to help keep all your body's tissues, including your skin, well hydrated.
Attention, thinking and memory problems
Changes to attention, thinking and memory can be grouped under cognitive impairments, and can be caused by both chemotherapy and radiotherapy. Cognitive impairments can also result from other medications taken to help early- and late-effect side-effects of cancer treatment. Brain fog is real!
Cognitive impairments can be managed through medication and cognitive rehabilitation and training, such as exercises to improve memory and problem solving. Learning a new language works really well as a cognitive rehabilitation tool. Exercise, including gentle walking, gardening, swimming etc, also has important physical and cognitive benefits.
Early Side-Effects
Side effects experienced during treatment and in the months immediately following treatment, often referred to as the recovery period.
Late Side-Effects
Side effects that may occur from one year to many years after treatment.
What To Expect

Please join our private Facebook Group to get support and advice from fellow patients and carers
Want to get involved in Oracle´s aims and goals?
If you have direct, lived experience of Head and Neck cancer as a patient or carer, or you may just be passionate about helping us ensure that there is greater understanding of these cancers in the wider population and that all voices are represented.

