Please join our private Facebook Group to get support and advice from fellow patients and carers
Immunotherapy for head and neck cancers
Immunotherapy for head and neck cancer - background
Immunotherapy for head and neck cancer patients in the UK is only offered to people who have advanced head and neck cancer, i.e. whose head and neck cancer has been treated once but has now come back. Advanced cancer may be recurrent (if it has returned to the original site and surrounding lymph nodes) or metastatic (often called stage 4 cancer), if it has spread elsewhere in the body that is different from the primary tumour location.
Immunotherapy works by stimulating or enhancing the body's immune system to fight cancer cells. Unlike traditional treatments like chemotherapy, which directly attack cancer cells, immunotherapy helps the immune system recognize and target these cells more effectively. There are many classes of immunotherapy drugs, with the most common ones used to treat advanced head and neck cancers belonging to a class called ‘checkpoint inhibitors’. Drugs belonging to this class approved by the UK’s National Institute for Health and Care Excellence (NICE) include Pembrolizumab (Keytruda) and Nivolumab (Opdivo)). These drugs work by blocking proteins that prevent T cells from attacking cancer cells.
The field of immunotherapy is rapidly evolving, with new research and potential treatments emerging regularly. Patients considering immunotherapy should discuss their specific case with their oncology team to understand the most current treatment options available to them in the UK healthcare system.
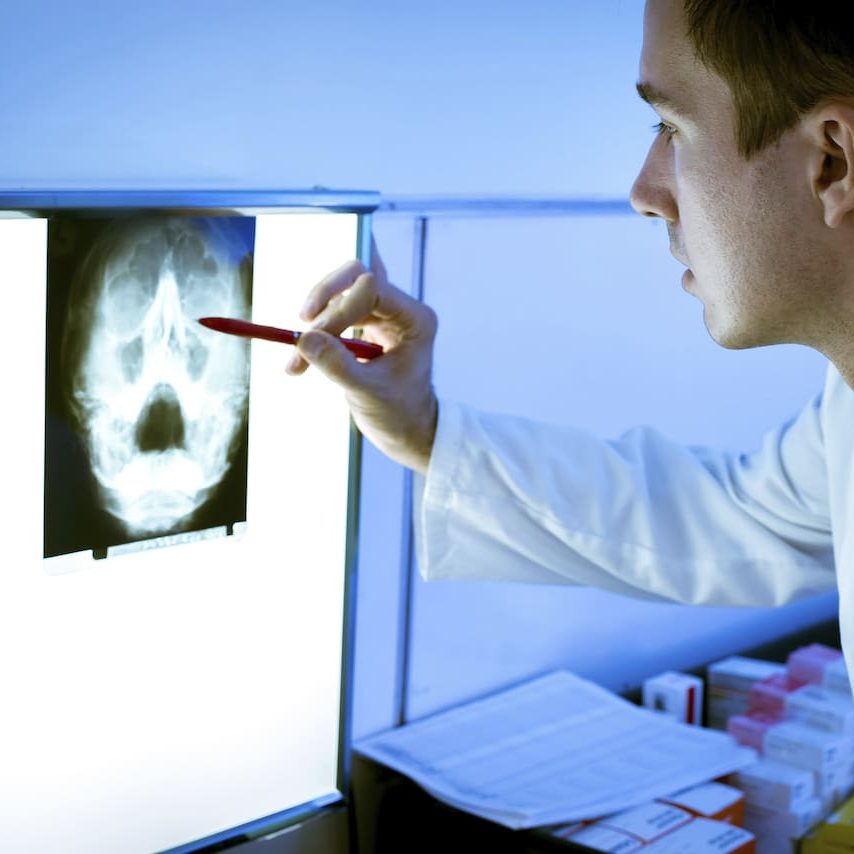
Suitability tests and biopsies
Not all all patients respond to checkpoint inhibitor drugs, and to determine those who are most likely to be responsive, a biopsy of your tumour will be undertaken. The biopsy looks to see if your tumour cells have a special receptor protein called PD-L1, as this is the partner protein of the checkpoint protein PD-1 present on the surface of your T cells. Block the connection between PD-1 and PD-L1, and you block, or inhibit, this particular checkpoint. Biomarkers like PD-L1 expression are sometimes used to help predict which patients might benefit most from immunotherapy treatment.
General Information
A quick overview of what to expect
Chemotherapy / Radiotherapy
A quick overview of what to expect
Surgery
A quick overview of what to expect
How Immunotherapy works
This video explains really nicely how T cells recognise cancer cells, but also how cancer cells can evade detection through signalling to immune checkpoints.
Starting immunotherapy treatment
The drug is initially given intravenously , in a hospital setting, either every 2-3 weeks or every 6 weeks, depending on the dose.
Immunotherapy drugs such as Pembrolizumab are licensed in the UK for a maximum of 2 years. Treatment can continue for up to two years therefore, or until disease progression or unacceptable toxicity. A few days before each immunotherapy infusion, you will have blood samples taken to check on the numbers of red and white blood cells, alongside other tests (e.g. for thyroid function), to make sure that you are well enough for the next infusion.
Side effects of immunotherapy
Generally, there are fewer side effects with immunotherapy than traditional chemotherapy. Common side effects may include fatigue, skin rashes and diarrhoea. However, although severe side effects are less common, they can be very dangerous and require urgent medical care. These side effects may include autoimmune driven inflammation of the liver, heart, lung, pancreatitis, kidney failure, and bowels. Rarely, anaphylactic shock may occur.

Conclusions about Immunotherapy
Immunotherapy drugs may be given alongside other treatments, such as chemotherapy, or surgery. However, the the field of immunotherapy is rapidly evolving, with new research emerging regularly for example, research is ongoing to identify new immunotherapy targets and to understand why some patients respond better than others. There is also interest in using immunotherapy earlier in the treatment course, potentially even as first-line therapy in some cases. Clinical trials are ongoing investigating different types of combination therapies .
Patients considering immunotherapy should discuss their specific case with their oncology team to understand the most current treatment options available to them in the UK healthcare system. Several UK institutions are involved in clinical trials exploring new immunotherapy drugs or combinations for head and neck cancer. We recommend that you discuss all options with your oncology team.
Exercise and Rest
Exercise and rest are crucial for your treatment to be successful. Your body is going to take a significant amount of punishment from the treatment so be prepared to have daytime sleeps and rest. Regular exercise when you feel most perky in the day is good for your mental and physical health even if it is simply walking around the block once a day.
What To Expect