Types of Head and Neck Cancer
Thyroid Cancer
On this page
Head&Neck Cancer Types
Cancer Description
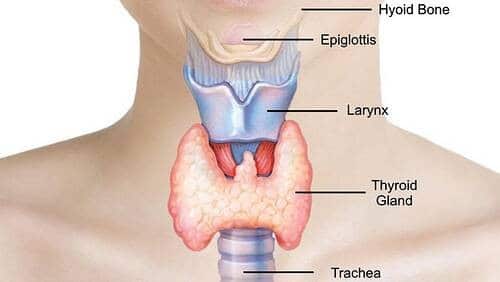
The thyroid gland is a small gland in the front, lower part of your neck, just below the voice box (larynx). It makes and releases hormones that regulate the ‘body clock’ (metabolic rate, growth and development). Thyroid cancer affects almost 4,000 people each year in the UK. Women are more likely to get it than men and it is a cancer that is seen in younger age groups.
There are different types of thyroid cancer. The most common types are papillary and follicular cancer and generally having a good prognosis. These types of thyroid cancer together are called ‘differentiated thyroid cancer’ (DTC).
Papillary
This is the most common type of thyroid cancer. It is usually slow-growing and more common in younger age groups and women.
Follicular
This is a less common type of thyroid cancer. It is mostly found in middle-aged people.
Medullary thyroid cancer (MTC)
This a rare type of cancer. It can sometimes run in families and is associated multiple endocrine neoplasia.
Anaplastic thyroid cancer
This is a very rare type of thyroid cancer that is fast-growing and aggressive.
Thyroid lymphomas
This starts in the lymph tissue of the thyroid. The lymph tissue is part of the body’s lymphatic system. Most thyroid lymphomas are a type of non-Hodgkin lymphoma (NHL).
Symptoms of Thyroid Cancer
Symptoms include: a lump and/or pain in the front, lower part of your neck – the lump usually feels hard, slowly gets bigger and is not painful, a hoarse voice, a sore throat, a cough, difficulty swallowing or breathing.
Common Treatment Approaches
The treatment for thyroid gland cancer typically involves a combination of treatment methods, and the exact prognosis depends heavily on the stage at diagnosis. Your consultant will describe your specific treatment and prognosis. The information below is for illustration purposes only;
- Surgery. This is primary treatment for most thyroid gland cancers. It involves either partial (Lobectomy) or total removal of the thyroid gland (total thyroidectomy). It possibly may include surrounding tissue and could include lymph node removal if cancer has spread. Much depends on the stage and size of the affected area, laser surgery can be used to accurately removal the tumour.
- Radiotherapy. Often used after surgery to kill remaining cancer cells. Sometimes used as primary treatment if surgery isn’t possible and may be given before surgery in some cases to shrink the tumour. The treatment may be combined with chemotherapy (chemoradiation). Some patients are asked to take a radioactive iodine pill but it is only effective for certain types of thyroid cancer.
- Thyroid Hormone Therapy. Used after thyroid removal where patients take synthetic thyroid hormones. This helps maintain normal metabolism and can help prevent cancer recurrence.
- Chemotherapy. Rarely used after surgery or radiation. May be recommended for advanced cases.
Your consultant will evaluate your overall general health at the point of diagnosis looking at the following aspects; the cancer stage at diagnosis, age and lifestyle. The prognosis for thyroid cancer is generally very good, especially when caught early. Most thyroid cancers are highly treatable, with five-year survival rates over 98% for localized cancer of this type.
The consultant will have regular check-ups with you for at least 5 years after treatment. Many patients can return to normal activities, though some may experience lasting effects from treatment, such as dry mouth or changes in swallowing function. See Post Treatment side effects.
Useful Links
Suggested additional sites that may offer helpful information:
Patient Stories
We don't have any patient stories currently for this type of cancer. Please get in touch if you would like to share your patient story.
Please join our private Facebook Group to get support and advice from fellow patients and carers


