Difficulty swallowing and her cancer diagnosis journey -Kelly
“I had to fight to stay alive.”
Kelly Watson, 43, knew something wasn’t right when she began to choke on food – a known symptom of cancer. So why did it take more than three months for this East Yorkshire mum to get a diagnosis and begin treatment? Here she shares her full story with Oracle Head and Neck Cancer UK, and thanks the dream team that got her through this terrible time.
Anyone could understand if Kelly Watson wanted to put cancer behind her. But these days, the Yorkshire mum is more interested in speaking up.
“Postcode lottery” situation needs more people to speak up
Her gruelling treatment for head and neck cancer finished in January this year, and it took months to feel even a little bit better. But even worse was the fight to get a diagnosis, when Kelly knew something was wrong. Alongside around a third of cancer patients waiting too long according to NHS targets, Kelly faced significant delays, causing her and her family huge amounts of stress and allowing the tumour to grow.
Kelly explained: “I felt like I had to fight to stay alive. To fight and fight to get the care I needed. Now I want to help hold the government accountable for the lack of funding and the cancelled appointments. I am not the only one and I want future patients to get good care, no matter who they are or where they are. At the moment, it’s a postcode lottery. And if we don’t speak up, nothing will change. People never hear about head and neck cancer and they don’t think it will happen to people my age. We have breast cancer storylines on Emmerdale, but nothing about head and neck cancer.”
Kelly’s trials began in August last year (2023) when her glands became swollen and she began to choke on food. She could not get an in-person appointment with a doctor and accepted a phone appointment instead. She was given antibiotics and after looking in the mirror, saw she had a lump in the back of her throat that looked like a large ulcer. Feeling deeply that something was wrong, Kelly visited Outpatient services where she was told it was a swollen tonsil.
Kelly said: “When they said that I asked: ‘Are you sure? Are you really sure that’s what it is?’ and they said yes. But I know my body and I knew something wasn’t right. The lump looked abnormal to me, and I was choking on food.”
Diagnosis delays
A week later, with no improvement, Kelly again asked for a doctor’s appointment and was told again it was an infection but that she would be referred to the Ear, Nose and Throat Department (ENT) of her local hospital ‘to be on the safe side.’
That night, Kelly had a panic attack, again feeling scared and that something was badly wrong as she was finding it difficult to swallow.
She said: “My dad took me to hospital, and I saw someone from ENT who said I had a lump on my epiglottis (the flap that covers the trachea during swallowing so that food does not enter the lungs) and that it looked like a cyst that needed to be removed. They said it didn’t look like cancer, but booked me for a CT scan anyway.”
On August 30th, Kelly had her CT scan. On September 11th she was sent to have the lump removed (she thought) and then sent home to recover.
Kelly said: “I thanked them because I thought they’d removed a cyst. They told me they’d done a biopsy because there was a lot of blood and that I would get the results in 10 days. I didn’t feel it was explained well. When I looked in my mouth and could still see the lump I started to panic because I thought they had taken it off.”
Life-changing news, and more delays
Ten days later (on September 21st) Kelly had still not had any results from the biopsy or CT scan. Later that day she received a call back from a consultant that seemed to confirm her worst fears.
She said: “They told me there were still no biopsy results yet, but the CT scan showed what looked like cancer. They said they were sorry and it wasn’t what they’d hoped for. They also said they could not see me for an appointment because they were going on holiday, but they would arrange an appointment with someone else.”
Despite the seriousness of the situation, Kelly’s next two appointments were cancelled the day before and on the day, respectively.
She said: “I went through all sorts of emotions. I was scared, worried, upset. In my mind I had cancer and there was no support other than my family. They didn’t know what to think. I feel like I was left in limbo. I was also in a lot of pain and could not swallow properly.
“I knew the strikes were happening but was told my appointments were cancelled because staff were on holiday, underqualified or off sick.”
Squamous cell carcinoma diagnosis
Kelly’s next appointment was on October 5th and she was formally diagnosed (from her CT scan and biopsy results) with T2 (T2 means the tumour is small and has not started to spread) squamous cell carcinoma. But her wait for treatment was not over.
She said: “I then did not see the oncologist until October 24th but I did think when I saw them it would be all systems go. It took until December 6th to actually start treatment.
While waiting, Kelly was sent to the Maxillofacial Unit department to see if she needed dental work which is standard procedure for head and neck cancer patients. She was told to either find an NHS dentist or pay to go private and have two fillings done.
Kelly said: “I was beside myself at this point. I didn’t have a dentist, and I didn’t have the money to go private. I was waiting for my Universal Credit to start. I rang every single dentist in the area. Eventually I found one 20 miles away who put me to the top of a waiting list of 300 when I explained why I desperately needed the work.
“I spoke to my Clinical Nurse Specialist, and she said to try my hardest but if I couldn’t get a dentist they would still go ahead with my cancer treatment. But that would have put meant a much higher risk of some terrible side effects.”
Waiting for cancer treatment
Kelly continued: “While I was waiting for treatment, I felt the cancer was just being left to grow. My Cancer Nurse Specialist was trying to reassure me not to panic but I couldn’t turn my neck anymore. It was really scary. It would have helped so much to be treated on time. I was diagnosed with T2 cancer, and they said it was T3 by the time I started treatment so it had got worse.”
Kelly had a radiotherapy mask fitted and feeding tube inserted through her stomach in preparation to start treatment. She then began 30 days of radiotherapy and 6 weeks of chemotherapy, on December 6th, more than three months after her CT scan to rule cancer in or out. She was told that surgery was not an option as the tumour was too large to get a good margin clearance.
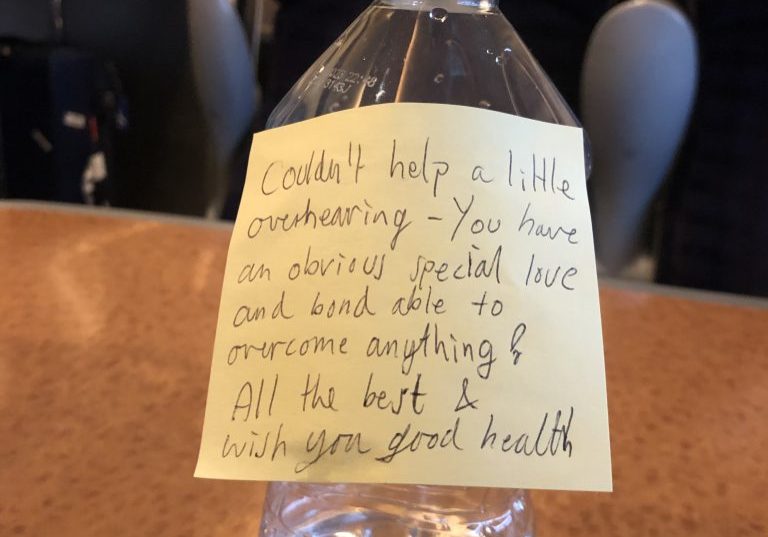
Her uncle drove miles each day to take her to treatment, and her mum came with her for moral support. Kelly says she is ‘beyond grateful’ for the help she had from her family. She also wants her treatment team to be acknowledged for the care she received.

Team effort for Kelly
Kelly said: “Hats off to the radiotherapy team that treated me, because they were amazing. The last two weeks the machines kept breaking down and they would stay until 9pm and work weekends even though it was Christmas, and I know they would have wanted to be with their families. They made it personal to me, remembered my name, greeted me warmly every day. They were so friendly I looked forward to seeing them and it made up for a lot of the bad experience I’d had.
“They gave 110% and at the end I took them biscuits and a card. They were so caring and when I saw them smiling it made me want to smile too.”
Kelly also received great support from volunteers Dani and Hazel from Oracle Voices, who have had head and neck cancer. They answered Kelly’s questions and put her in touch with another woman called Debbie who quickly became a good friend. Kelly was then referred to support from charity Young Tongues, because of her age, and Kelly found the charities’ active Facebook group a valuable source of support.
End of treatment, recovery and speaking up for others
After finishing treatment, Kelly was told to go home, rest and watch box sets.
She said: “It was another huge battle to recover from treatment. I was told two weeks and it took me 12. I’m still not back at work due to the late effects. I have feeding issues, very low energy and very little saliva which is horrible. When I swallow I am getting food and drink in my lungs.
“I have a friend who has been through treatment for head and neck cancer treatment under a different NHS Trust and she has been able to see a lymphoedema nurse for a regular massage.
“I was told to go and buy a small paint roller and do it myself with that.”
Everyone should get a high standard of care, on time
Kelly’s message is clear. She wants to see every patient offered the same high standard of care, on time.
“I strongly believe that treatment and aftercare should be the same across the board. It should be fair across the country and not depend on where you live.
“That should apply to dentistry too.
“My treatment team encouraged me to make a complaint about the delays in my diagnosis, but I don’t know how to complain or who to. My aim now is to tell my story because I don’t want anyone else to face these delays. Cancer care should not be about doing the bare minimum. It shouldn’t be held up by a lack of funding. People should get good care whoever they are and wherever they are.
“I want people to know what it’s like behind the scenes for people with cancer – too much gets glossed over. I think everyone should feel that the system will care for them if the worst happens. It shouldn’t hang on the funding.”
Published with sincere thanks to Kelly Watson: and Barbara Fountain from Young Tongues.
If you´ve been affected by Kelly´s story
Let’s all take action to prioritize our health and raise awareness for early detection.
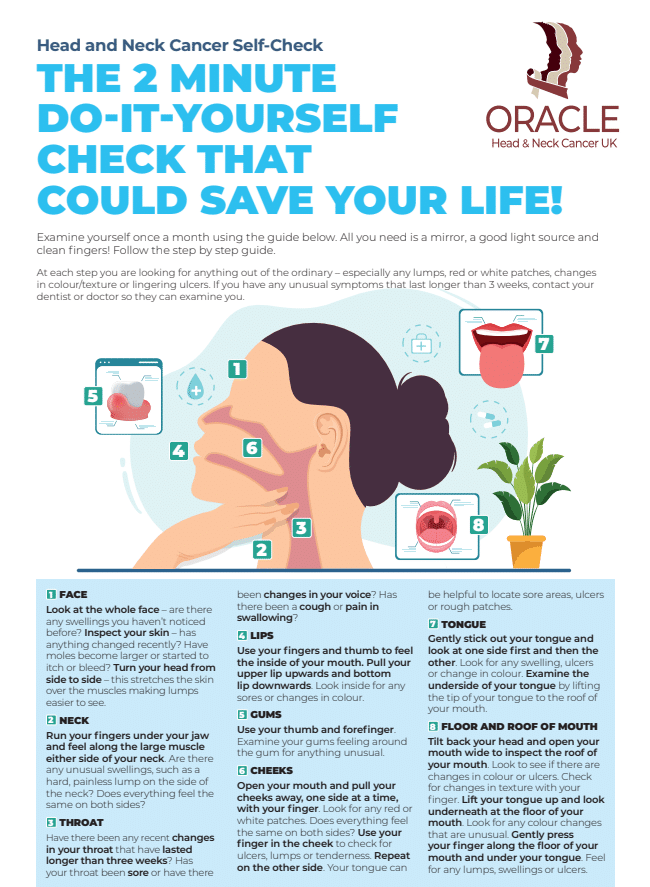
If you´re worried about changes in your voice, neck or mouth please refer to our simple “home check” guide.
See also other patient stories to hear about other people diagnosed with Head and Neck Cancers.
Have you got a symptom, are you being diagnosed, going through treatment, or a friend/carer of someone who is?
Please join our private Facebook Group to get support and advice from fellow patients and carers.
Patient Stories

Suzie Cooke – a lesson in not taking ‘no’ for an answer

Nigel Lloyd-Jones – being told “you have cancer” is life changing

Belinda Gilfoyle – a slow recovery and learning to stay positive

Salivary Ductal Adenocarcinoma news “hit me like a train”