My earache cause was a sign of advanced tongue cancer
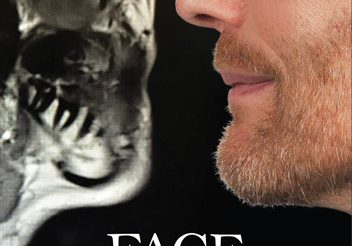
To see him now, you’d be hard pressed to imagine what Harvey Deaton has recently been through. He’s fit and healthy and enjoys spending his time between the UK and his holiday home in Spain. He’s lucky to be doing any of this. For months Harvey was told that repeated bouts of pain in his left ear were due to an infection – in fact ear ache was a sign of advanced tongue cancer.
Ear ache mis-diagnosed by GP and ENT
Harvey had been back and forth to his GP for help with the ear pain but despite trying antibiotics and ear syringing, six months on he was still suffering. It was during a routine dental appointment that his dentist noticed a ’red patch’ in his mouth that wasn’t healing.
She advised him to see a specialist in conditions affecting the head and neck who within minutes had diagnosed the true cause of his earache and the sore in his mouth – cancer of the tongue.
Harvey, from Kippax, in Leeds, says: ‘They told me ear pain was a classic sign,’ he says, ‘but I had no idea constant ear pain can be a sign of head and neck cancer. It was caught in the nick of time – I’m lucky to be here.’ By the time he was diagnosed, Harvey, 59, a former BT manager who is married to Helena, 56, had stage four cancer which had spread under his tongue to one of his lymph nodes.

“Huge surge” in cases is expected
Around 12,800 people in the UK are diagnosed with head and neck cancer each year, according to Cancer Research UK but cases have been rising – by as much as 30 per cent each year – and that ‘huge surge’ is expected to continue says Dr Oladejo Olaleye, a consultant ear, nose, and throat surgeon at the Leicester Cancer Research Centre and ambassador for the charity Oracle Head and Neck Cancer UK.
Head and neck cancers are those affecting the throat, voice box, nose and sinuses, tongue, tonsils, gums, lips, jaw bone, cheek bone, cheek, neck lumps, salivary glands, and the thyroid area. Although most cases occur among those in their mid to late 60s, the numbers are rising ‘alarmingly’ in younger men and women too says Dr Olaleye.
HPV is driving the increased numbers of cases
The recent increase in head and neck cancer cases is largely attributed to high-risk strains of the Human Papillomavirus (HPV), a common virus linked to cancers in areas such as the tonsils and base of the tongue. These cases are now more prevalent among younger men, who may experience symptoms like a persistent sore throat or a lump in the neck. Dr. Olaleye emphasises the importance of awareness, as early detection can significantly improve outcomes for those affected by HPV-related cancers.
It’s crucial to address a common misconception: contracting Human Papillomavirus (HPV) does not require sexual activity. HPV can spread through non-sexual means, such as skin-to-skin contact, meaning anyone can be at risk. This fact underlines the importance of preventive measures and awareness for everyone, regardless of lifestyle. By understanding HPV’s broader transmission routes, we can help ensure that information about HPV vaccination remains accurate, encouraging widespread vaccine uptake.
‘Although HPV vaccination was introduced (for teenage girls in 2008, but also for boys in 2019) and is expected to reduce cases of head and neck cancer (particularly those of the tongue and back of the throat), the full impact ‘won’t be seen for several decades as these cancers typically develop later in life,’ he adds.
There are however other risk factors for head and neck cancers, including smoking and excessive alcohol consumption.
Ear pain is a referred pain due to shared nerve pathways
Symptoms of head and neck cancers can include a persistent sore throat (or other type of pain in throat or mouth area), a neck lump or swelling, lump or ulcer on the lip or in the mouth that does not heal, changes in voice or hoarseness, painful swallowing or difficulty swallowing and earache or ear pain.
‘Ear pain can be a sign of certain head and neck cancers, particularly those affecting the throat or base of the tongue, due to shared nerve pathways,’ says Dr Olaleye.
‘Most of the time ear pain is caused by other conditions like infections or jaw joint disorders but if there is unexplained ear pain for three weeks or more, it should be investigated thoroughly.’
He stresses that it’s also vital for anyone who has symptoms including; unusual lumps on the tongue, whiteish or red patches on the tongue/cheek, non-healing ulcers, and persistent sore throats, that last more than three weeks to see their GP or dentist. Survival rates for head and neck cancers are generally lower than for some other cancers, such as breast cancer, says Dr Olaleye, partly because the anatomy of the head can make surgically removing some cancers challenging.
Hence while around 70-90 per cent of patients with lip cancers, which are easily visible and accessible, will live five years or more only 40 per cent of patients with more inaccessible cancers such as hypopharyngeal cancers which develop in the lower throat behind the voice box, live five years or more. In comparison, the overall survival rate for breast cancer is around 90 per cent.
Remedies and tests for ear ache failed to find the real problem
Harvey’s earache began in August 2022 and when his pain failed to improve despite antibiotics and ear syringing Harvey by October was on the maximum daily dose of paracetamol returned to his GP. This time he was given a nasal balloon device to try – the idea being that breathing out through your nose to fill the balloon with air helps to equalise pressure in the ears. This too didn’t work.
Some weeks after this, in November 2022, Harvey burnt his mouth on some hot soup – but the wound wouldn’t heal. By now he was alarmed – ‘I knew in my gut something was wrong.’
In January 2023 he insisted that this GP refer him to a specialist. He saw an ENT consultant at a private clinic through the NHS. Tests including; hearing tests, an endoscopy to check for abnormalities in his throat and the eustachian tubes (connecting his middle ear and back of his throat) all cam be clear.
Routine Dentist appointment was key
In April, he had the dental check-up near the Spanish holiday home he owns in Cabo Roig on the Costa Blanca with his wife Helena – and happened to mention the burn that hadn’t healed. The Spanish dentist examined it carefully, appeared concerned and said there was an infection at the base of his tongue. When Harvey returned, as she’d asked him to, three weeks later, she examined the ‘red patch again’ and said it looked more inflamed than before.
When Harvey mentioned his ear pain, she advised him to quickly book an appointment with a private maxillofacial consultant – whom he saw on his return to the UK.
After examining Harvey’s tongue and listening to his symptoms, the consultant simply said: ‘I know what this is. It’s cancer. I’ll put you back into the NHS as this is going to be expensive to cure!’ After being ‘fobbed off’ for so many months, Harvey was ‘stunned’ that his problem could be diagnosed by an expert ‘in seconds.’
The cancer was situated under his tongue but a phenomenon known as “referred pain” meant that the pain could also be felt in his ear. As the mouth and ear share common nerve pathways, pain signals from one area could be felt in another. The diagnosis was confirmed by a scan and a biopsy which stated that it was caused by HPV.
Radio and chemotherapy treatment as surgery was too tricky
Harvey was referred back to the NHS and had 35 radiation therapy sessions on his head and neck and 3 doses of chemotherapy over a gruelling seven weeks. He had to have 5 teeth out to reduce the risk of dental complications in later life, and had a tube fitted into his stomach for feeding.
‘The treatment was brutal as its effects are cumulative and the pain in my mouth and throat was so intense. I couldn’t have surgery because the tumour was 4cm wide and in a difficult place to operate under the base of my tongue. I had liquid morphine which caused acute constipation and was tube fed throughout treatment and for 4 weeks afterwards. It was very hard for me and for Helena watching me go through it.’
He lost a stone and a half, dropping from 13.5 stone to 12 stone (he is 5 ft 10) during the three months of treatment.

While surgery wasn’t an option for Harvey, it can be effective for early-stage cancers, removing the tumour completely, however more advanced cases may require reconstructive surgery in the head and neck area using muscles and blood vessels from elsewhere in the body.
Dr Olaleye says that while improved diagnosis rates are urgently needed ‘it’s not only about survival. It’s also about quality of life – a lot of patients who survive head and neck cancer go on to have very challenging lives post treatment if they are diagnosed late and their cancer has spread due to breathing problems and often complex reconstruction.’
For some, extensive surgery can involve removing their tongue and/or voice box, he says.
I am lucky to be here!
A year after his treatment ended, Harvey is cancer-free but still being monitored by his consultant. He volunteers for the head and neck cancer charity Oracle Head & Neck Cancer UK, running their website because he wants to ‘give something back.’
‘I now know that ear pain is a classic sign of head and neck cancer. Yet my GP and ENT specialist I saw never mentioned this. That meant my cancer could grow to stage four,’ Harvey said.
He remains grateful however that his cancer was caught. ‘I am so lucky to be here. I am sharing my story so that other people know the signs to look out for.’
If you´ve been affected by Harvey´s ear ache and tongue cancer story
Let’s all take action to prioritize our health and raise awareness for early detection.
If you´re worried about changes in your voice, neck or mouth please refer to our simple “home check” guide.
See also other patient stories to hear about other people diagnosed with Head and Neck Cancers.
Have you got a symptom, are you being diagnosed, going through treatment, or a friend/carer of someone who is?
Please join our private Facebook Group to get support and advice from fellow patients and carers.
#headneckcheck
Regular self-checks play a vital role in the early detection of Head and Neck cancer
Patient Stories

Suzie Cooke – a lesson in not taking ‘no’ for an answer

Nigel Lloyd-Jones – being told “you have cancer” is life changing

Belinda Gilfoyle – a slow recovery and learning to stay positive

Salivary Ductal Adenocarcinoma news “hit me like a train”