Jono’s story
My name is Jon Organ, or Jono as I have been called my whole life. I am 58 at the time of typing. I have been married for 37 years, have four grown-up children and 11 grandchildren. In my work life, I worked for myself for many years. I consulted on construction and workplace health and safety, and also Equality, Diversity and Inclusion. Today I still teach and present on EDI in the workplace and race and social inclusion. Social injustice is still my biggest passion in life. I am the founder of Life after Lary, a support group for laryngectomy patients and carers that has over 2,000 members. I have paid roles with The Royal Marsden on their biomedical cancer research working panels as well as precision therapeutics and cancer treatment effects. I also have a lead role in The Royal Marsden EDI steering panel. I also have other paid roles. One is with NICE as a lay specialist for robotic-assisted surgery. Another is with Great Ormond Street Hospital in genomic medicine where I sit on two panels there, one being EDI. I also have roles with Sheffield and Birmingham universities in cancer research and treatment effects. I am an ambassador to The Throat Cancer Foundation and a very proud member of Oracle Voices. I have also recently taken a new role to work on investigating radiotherapy in a sitting position rather than lying flat.
My life has always been busy and I throw myself into my work 100%. In December 2021 I presented to my GP with the symptom of always being tired and falling asleep in the day. Something I had never done, but for a few months I just fell asleep. I put it down to a bit of long covid maybe. Bloods were taken and they showed I was very low on red blood cells and I was dangerously anaemic. An emergency blood transfusion was ordered and I felt better, for a short while. Investigations took place and I was told in early February 2022 that I probably had cancer and it was probably pancreatic; they just needed to find it. Further tests were carried out and by now I was short of breath. More investigations were carried out and I was told I had asthma on top of a possible cancer. Bloods were all indicating cancer but still no answers. Many scans were ordered: PET scan, MRI scan, CT, the works, plus further blood transfusions. At one point I even swallowed a camera pill to look for cancer. By April my breathing was worse than ever and I had also developed a hoarse voice. I was told the voice was a side effect of the steroid inhalers. Every scan possible, blood transfusions etc. continued and still no answers. On 1st November 2022 I had one last scan, or so I thought, and this showed nothing. At that point I was told that 100% I did not have cancer. My breathing and bloods were still bad and I was living on high-dose iron medication and my voice was now a whisper. I returned to my GP on 3rd November and demanded I have further investigations. At no point had I been given an endoscopy to look at the throat. At no point did I have further investigation as to why my breathing was so bad and had now been told I needed home oxygen. I stamped my feet and got very dramatic and my GP, more to get rid of me I think, arranged another two-week rule to see ENT. By this time you start to believe you are going mad and you kind of hope something is found, just to explain why you feel so ill. I felt so ill, as if I was dying. I saw ENT on 16th November 2022. This was my last hope I felt. By this time it was all put down to long covid but I did not accept that. You know your own body. I remember sitting there with my wife and the nurse was arranging files. One of them was about 8 inches thick. “Bound to be mine,” we joked. How much had I cost the NHS this year was unthinkable.

At 09:15 on 16th November 2022, Mr Arun Takhar, an ENT consultant and later my surgeon and now my friend, placed a scope through my nose to look down my throat. This took around 4 minutes. That was all. Four minutes after 12 months of being a professional patient. It was removed and with his hands on his knees he leant forward and said, “I am afraid you have advanced cancer and I would guess it’s stage 4. You have 60% of your airway blocked by the tumour and surgery is needed very soon.” FINALLY, an answer.
Not that I wanted that, but an answer. I asked how long it had been there and the guess was that it had been growing for many months… It was there all along. It had been missed again and again and again. More scans were ordered to pinpoint and stage the cancer. Also, a biopsy was taken during surgery. After all of the scans I was told the cancer was stage 3 and seven weeks of radiotherapy and chemotherapy and I would be cured. I needed one more ultrasound scan and a CT at The Royal Marsden Chelsea to arrange measurements etc. This was done on 12th December and I saw my team again on 20th December. All of a rush now because of the Christmas break coming up. I presented to The Royal Marsden in Sutton, Surrey on 20th December where I was told my final plan. It was stage 4 and had spread to the thyroid gland and blood vessels. Probably the lymph nodes as well but they could not be sure. The only plan now was a total laryngectomy. They would remove the whole throat, voice box, thyroid and 84 lymph nodes. They would borrow muscle from the chest and/or back to support the head. I would have a permanent hole in the neck to breathe through and a speech valve inserted between the trachea and oesophagus. I would be taught how to swallow, breathe and speak again.
Once surgery had been completed I would have six weeks’ radio and chemotherapy and the journey would be long and hard. My life would change forever. It had taken 12 months to get to this. Twelve months… I decided I would opt out and did not want my life to be like that. My options were explained: that if I refused the surgery I had four months at best, six months to live. With the surgery they hoped to give me five years but the first two of those years would be the hardest I have ever faced, physically and mentally. So, three years I thought, but it’s only a number. Maybe longer, I said to myself. Maybe 10. Who knows. I had three days to decide as the surgical teams broke for Christmas and my surgeon was not back until 9th January. If I decided against it then it would be a hospice. On the 11th hour of day three, on Friday 23rd December, I decided to do it. Eleven hours of surgery was planned for 9th January 2023. February 2023 radiotherapy and chemotherapy were planned. I remember during radiotherapy I asked for support for my mental health. I was told, “Mr Organ, I can put you on a list but you will either be dead or cured by the time you get to see anybody.” A story for another day.
Today, over two years later, it has been the single hardest thing I have ever done and on many occasions I thought about ending it. Many occasions. Even today I face more surgery in the coming weeks because of the radiotherapy. A laryngectomy is the biggest part of the journey but for me, like many others, the rads and chemo are worse. Many laryngectomy patients do not have any more treatment after surgery and go about their lives. Still a difficult journey but they seem to get on better. Those that do have the rads and chemo struggle badly. The surgery I face is to stretch the oesophagus and scrape to help me swallow. I will also have some scar tissue cut away that has been left from radiotherapy. Today I live in constant pain and still take opioids: morphine-based meds, and I also wear lidocaine patches on my shoulders and fentanyl patches on my arm. My feet and hands are numb and I have had 9 falls. I am an artist and it is hard to paint in detail with numb hands. I sleep upright in an electrical hospital bed as I am constantly sick because there is nothing left now to stop food reappearing. Also, I have no upper body strength to get me out of bed. The daily care of my stoma is a full-time job. I have no sense of smell and wear two hearing aids. My home has been adapted as I can no longer bathe and need help to dress and to shower. I wear a snorkel attachment to stop any water entering my stoma as I would drown. Food is a real challenge and many things including bread or cake, that I loved, I have not been able to swallow since surgery. Life is very different and very challenging now. Every single day. I also take 61 tablets a day including antidepressants. Thankfully my wife is a saint and my best friend. Without this support we as patients would not survive. I know I wouldn’t. Chemo has damaged my heart and liver as well and I now have kidney disease and heart disease. I am also registered disabled. Before all this I ran and cycled miles. I would often run 12 miles on a Sunday. Today, some days I cannot get out of bed. I recently climbed the last bit of Snowdon for charity. I got the train three-quarters of the way up and walked the last hour. I was helped up on either side and then spent six days in bed following that. Crazy.
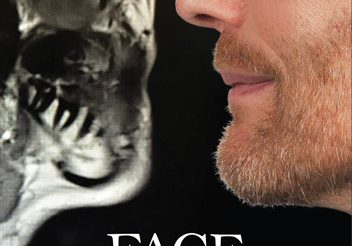
What keeps me going you may ask? Helping others is what I have always tried to do in my life. Those that life has left behind. Those that flee wars or persecution. Those that have no voice and now I can do it through lived experience. I have a website www.lifeafterlary.com and my video diary is on my Instagram lifeafterlary. I am also in the process of writing my book. A book of self-help and survival. It does not always happen to someone else. I am the someone else.
Try to light the way others are yet to tread. Your knowledge and the road you have taken is key to others’ survival.
Patient Stories

Suzie Cooke – a lesson in not taking ‘no’ for an answer

Nigel Lloyd-Jones – being told “you have cancer” is life changing

Belinda Gilfoyle – a slow recovery and learning to stay positive

Salivary Ductal Adenocarcinoma news “hit me like a train”