Jon’s persistent hoarse voice caused by cancer not asthma inhaler
Jon (56), a husband and dad of 4, experienced a persistent hoarse voice for over a year but put it down to the new inhaler he was taking. In November 2022, his world turned upside down and here he shares his story.
Hoarse voice symptoms – 7th November 2022
This is our story, and it starts well over a year before I was diagnosed when I started taking a new inhaler to help with an early diagnosis of emphysema. The inhalers side effects were a hoarse voice and yes, I did develop a hoarse voice. So, nothing was thought to be strange about it and life just carried on. Today a day after my birthday, a nurse from my local doctors called me to ask how things were going with my general health and to check on my breathing etc. She flagged the voice and sent me an urgent referral to see ENT. The following day a nurse from the local hospital called and asked a lot of questions. It would transpire that she was a Macmillan cancer nurse.

Diagnosis of cancer of the voice box – 16th November 2022
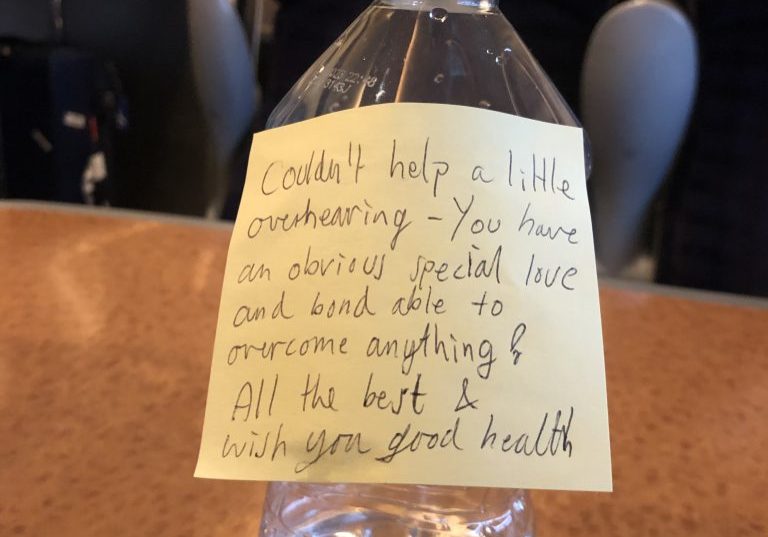
Today myself and my wife Nicky went to see Mr Takhar a day that will be forever etched in our minds and he looked and my throat and turned to me and said “you have cancer of the voice box.”
I replied: “give it to me straight doc will I lose my hair.” But seriously to hear those words are like being hit by a truck. I just did not want to show my initial shock. It sunk in pretty quick though as we both had a little cry in the office. At that point neither of us could even imagine how the story would unfold and the path it would take us. You do not really know at that point what is going to happen, but the shock is enough.
From there a whole host of scans and appointments. Once they have all the results in front of them, they call you in and tell you what the plan is and what the stage is. we were told initially it was stage 3 and radiotherapy and chemo would be the treatment. We were just waiting for the start date. Then we were told a pet scan would be needed and an additional ultrasound to get the exact location for the radiotherapy machine.
Treatment planning – 19th December 2022
At 3pm we were called to attend an oncology meeting at the Royal Marsden Hospital. This was the meeting, or so we thought, to tell us when the treatment would start. That is where they told us it was now agreed by the team it was stage 4 and beyond just radiotherapy and chemo. It was growing 40% over airway and into thyroid and a total laryngectomy would be the only course of treatment followed by 6 weeks radiotherapy and 2 courses of chemo. My first reaction was to swear at him and say no thank you. I had 3 days to decide because of the Christmas period and everybody being off. I was scared stiff thinking about it. I seriously contemplated no but Well I had no choice did I it had to be done. Do or die literally.
The operation was booked for 9th January at 9 am. It would last 9 hours and I would spend 24 hours in ICU with a 21 day stay in hospital. There was no way on gods earth I was staying in hospital for 3 weeks. Christmas was very different last year and the cancer and the operation was never far from our thoughts.
Surgery to remove the voice box – 9th January 2023
So, this was the day and it had arrived. I went into St Georges Hospital London to have life changing surgery. Nicky could not stay with me so had to leave me at the surgical day suite. It was a horrid feeling as she left but I could not show it. We both cried in our own space. The surgery was to remove the voice box. 92% of thyroid gland and 84 lymph nodes plus a procedure to leave me with a perm tracheostomy and TEP speaking valve put into place. TEP stands for Trachea Oesophageal Puncture. The TEP uses a one-way valve to let air pushed up from the lungs to pass through from the trachea and enter the oesophagus causing the walls of the oesophagus to vibrate as a new voice. This one-way valve if working as it should, will not let food or liquids pass through from the other way. It can be hard work at first getting the hang of it.
Recovering from the operation – 19th January 2023
I came round from surgery to be told I had covid 19. Wonderful. This meant 3 days in ICU in an isolation ward. I spent exactly 14 nights in hospital leaving at 7pm on the 14th night. Recovering from surgery was a hard road and not just because of the physical demands that the surgery put on me but the learning. learn to swallow, breath, eat and drink, and maintenance of the stoma plus learning to talk again.
On day 10 they take you for a swallow test. This test is to make sure water passes into your stomach and not lungs during treatment. Test was passed and puree food was allowed. On the road to recovery. The use of the products I must say was hardest bit of all for me and very scary. They provide you with a book and we went through this together with my SLT. Who were brilliant. I studied that book night and day and watched you tube videos. I had to get it right. There are so many products and so much that can go wrong it is a mind-blowing situation. But we got there. A completely new world to me and all are hard and all for different reasons. My whole life had been changed.
After surgery the tumour was biopsied, and they arrived at my bed to tell me the great news that all was got within the margins. It was very aggressive and had gone into the blood vessels but without surgery I would have passed away by end of June.
Life after surgery – 23rd January 2023
Once I was at home it was time to rest for 3 weeks. Rest is a bit of lie. There is still so much to learn. This I could do in my own time now and speaking to Atos who are at the front line was great. They have so much time for me and all my questions that I am sure they had before a thousand times.
After this 3 week rest I would have 6 weeks continuous radiotherapy and 2 doses of chemotherapy. The radiotherapy has many challenges regarding a tracheostomy. Because you are being in a way burnt, they have to take care of the tracheostomy. I went to a specialist hospital for this. I had a bit of burning and blistering inside but nothing too much. This took a lot of care. It became infected and very painful. Daily care is a must and a completely new routine to me. It was okay in the end. Things generally are.
Radiotherapy was hard. It made me really unwell and the last couple of weeks put me to bed. I will pass in future if I ever need it. I slept in the waiting room and slept in the ambulance home. The radiographers were great.
Chemotherapy I only had 2 doses so cannot speak on any real authority. What I will say with me it damaged nerve endings in my legs temporary.
Surgery itself has left me in a bit of a mess regarding shoulders and neck and pain. The surgeons borrowed muscle from shoulders and used in neck to amongst other things help hold my head up. Also, they lifted a lot of skin away from muscle etc to remove lymph nodes. As well as the small matter of putting a hole in my neck. My neck and shoulder pain could be long term who knows. Today I am still on strong opioids for pain and for how long who knows. I can never lift again I am told rupture the trachea if lifting heavy loads.
My nebuliser is my friend now. I hated it in hospital as it made me cough nobody there explained to me that this is the reason partly that we use a nebuliser. One to loosen secretions and one to help cough. Coughing gets rid of anything in the trachea and aids in breathing. I tend to nebulise 3 times a day, but I know when I need to. Sniffing has gone so a runny nose is an ongoing issue. I no longer have a sense of smell which I miss so much.

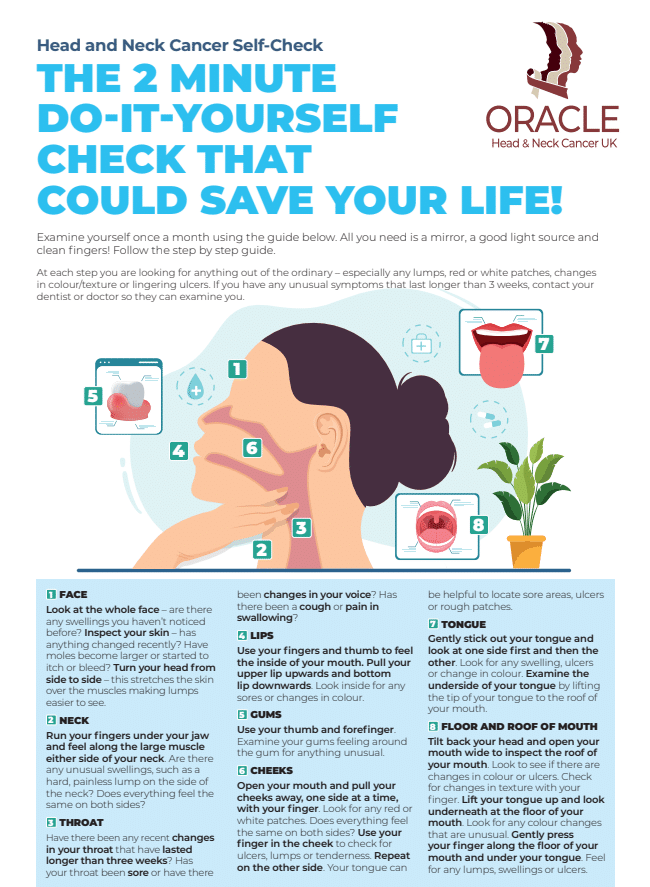
Jon highlights the importance of being aware of the signs and symptoms of Head and Neck cancer, and the importance of going to your doctor if they persist for longer than 3 weeks.
ED – Following Jamie Theakston´s announcement on Instagram of his treatment for Laryngeal cancer, Jon was interviewed by The Daily Star and offered advice and support to Jamie and his family.
Patient Stories

Suzie Cooke – a lesson in not taking ‘no’ for an answer

Nigel Lloyd-Jones – being told “you have cancer” is life changing

Belinda Gilfoyle – a slow recovery and learning to stay positive

Salivary Ductal Adenocarcinoma news “hit me like a train”