Tongue cancer surgery and radiotherapy – Stessy´s advice
Stessy Haberfield´s words of warning
Stessy Haberfield has very kindly shared her patient story to help other patients and carers coping with tongue cancer surgery and radiotherapy. Her cancer diagnosis happened in 2020 during the COVID 19 pandemic making her cancer journey much more tricky to navigate. She has been cancer free for 4 years now..
Please note – this is written from a UK perspective. It is a general guide only based on Stessy´s own experience. Every surgeon and hospital across the UK has different policies to match your specific case.
The following IS explicit – nothing is held back, so consider this before you continue reading.
Remember that it’s YOUR body and your operation, so no question is too silly. If in doubt, ask for a thorough explanation. Importantly second opinions are always allowed, but don’t hold up your surgery unnecessarily.
These sections are written in Stessy Haberfield´s own words.
Getting a diagnosis
If you’re here, it’s likely that you or the person you´re caring for will already have received a cancer diagnosis. You may or may not have been expecting it, but either way, it’s still something that needs to be processed; and that can take time too. Some people find it difficult to tell their families and friends. Others will be completely open from the outset.
There’s no right or wrong.
For me, once I’d got my head around it, I told my entire (social media) world.
If you are struggling, do reach out to Oracle people and the support groups they advocate.
This is a rough ride, but it is absolutely doable!

Biopsies
Pretty unpleasant, but this is currently the only fool-proof way to get a sample that can be properly analysed. I’ve had stitches burst on 2 occasions and it had to be re-stitched which was horrible. The best advice is to dose up on painkillers BEFORE you go in.
MRI, Ultrasound and CT Scans and Surgical Planning
If your biopsy has come back with a “positive” result of Oral Squamous Cell Carcinoma (OSCC) then the next stage would usually be for an MRI, an Ultrasound Guided Biopsy on the lymph nodes in your neck (that one doesn’t hurt) and a CT (including chest to check for any possible lung nodules).
After reviewing your scans with Multi-disciplinary team colleagues – including other consultants and Radiologists, your consultant/surgeon should have an idea about the extent of the tumour meaning that they can develop a plan. Most back of the tongue tumours are not operated on but are treated with Radiotherapy and possibly chemotherapy, particularly if there is lymph node involvement.
For many tongue cancer patients surgery is the first line treatment, but occasionally chemotherapy or immunotherapy might be suggested beforehand to shrink the tumour. Radiotherapy is not normally given before surgery as this makes healing much more difficult.
Tongue cancer surgery – the technical speak
A “partial” glossectomy is the removal of well below half of your tongue; hemiglossectomy – approximately half; total/subtotal glossectomy – nearly the whole lot!
Everybody will be different, but clearly, the size and location of the tumour will dictate whether or not your tongue needs to be reconstructed. A partial glossectomy typically takes 4 – 5 hours, with a 3 – 5 day hospital stay; if you need a reconstruction, this can increase to 10 – 12 hours and a hospital stay of nearly 2 weeks. At the same time, it is almost certain that you will have a “neck dissection” either on one side, or both.

Even if your lymph node biopsy is clear, it is nevertheless the most likely area for potential spread of stray cancer cells. This involves opening up your neck and cutting out the majority of your lymph nodes. This can cause swelling (lymphoedema) after surgery as your lymph no longer has an easy path to be drained from your face & neck. It can usually be managed with massage and exercise.
If your tumour is particularly big, or in an awkward position, you may need to have a “split jaw” to allow for better access. A zig-zag pattern is incised into your jaw below your lip. Whilst certainly invasive, the scars that I have seen have repaired remarkably well.
Reconstruction of the tongue
The donor site for a reconstruction is usually the inside forearm from your non-dominant arm known as a Radial Forearm Flap (RFF). The blood vessels are usually relatively easy to extract. If a small amount is needed, the skin may be pulled back together; a larger amount may need a “patch” from elsewhere – typically your tummy. Your arm will be out of proper action for a little while and there will be some significant scarring but it will fade with good care.
Some surgeons use the thigh or the calf called a Medial Sural Artery Perforator (MSAP) – that was me – or even parts of the shoulder or elsewhere. The flesh of the calf can be pulled together BUT the blood vessels are usually smaller & therefore more difficult to harvest. The blood vessels from the “flap” can then be plumbed into your own blood vessels through the space under your neck created by the neck dissection.
My tongue cancer surgery – in practice
Before surgery – eat! Try to load up in protein. if you’re able, in order to aid healing. The Nutribullet was my friend!
Be prepared
Buy some extra pillows, prepare and freeze some soups; stock up on soft foods for your discharge – yoghurts, porridge, eggs, custards etc. etc. You WILL need help on discharge. DO tell your “loved ones” JUST HOW MUCH HELP you will need. You will be knackered and helpless for a little while.
Packing things for hospital
Everybody has things they really like to have. I’d say essentials are phone, tablet/iPad, headphones, charger cables (and maybe a spare), slippers, a shawl, lavender oil, lip salve, moisturiser and toiletries, all your usual prescription meds. Your own nightwear – either pyjamas with buttons or a loose fitting, strappy nightie. I’d accidentally bought a maternity one with buttons at the shoulders which turned out to be ideal once I felt well enough to get out of my hospital gown!
Some very loose clothes. Books and puzzles – maybe! Pad of paper and pen – although I ended up just typing into my phone
The big day – operation day
I recorded my voice. The usual pre-op no eating stuff. I printed out a list of my existing meds and other issues (contact lenses, dodgy joints) and put copies EVERYWHERE for surgeon, anaesthetist and nurses.
I had some nice felt tip marker pen on my leg and my neck to mark out the intended incision locations. Then ….. I came around (apparently) at about 9.30 that evening. I recall having a button to press for morphine on demand. You’ll probably have this for around 24 hours. I had nasal intubation (up my nose) but most surgeons/anaesthetists seem to use a tracheotomy. That avoids any anxiousness for them about the airway being too swollen, but it’s also another incision that needs to heal.
I’m told that this is one of the most unpleasant aspects of the operation. I was very fortunate that my team does not tend to use them unless absolutely necessary, but from what I can gather, they key thing is – to relax and your body will do it for you. By next morning in ITU the meds had made me sufficiently stroppy to demand my mobile – NOW – so I had music and my headphones and told the world I was still alive!
Immediately after the operation an “NG” (nasogastric) tube will be placed. Most people have no recollection of this, but I do have a vague memory of briefly coming around! The tube goes directly down into your stomach and it is how you will be “fed” – depending on your operation and the hospital protocol. All medication also goes through the tube and honestly it can be rather unpleasant
The nurses will need to test the pH of the fluid at the end of the tube before starting a new feeding session as it MUST be sitting in the acid in your stomach to confirm that the end hasn’t actually moved and shifted into your lungs. I had problems with this and had to have it pushed further in under X-ray.
Top tip – lying on your side can sometimes get the tube end to sit in a nice pool of stomach acid 😁
You will also have a catheter until you’re mobile and a number of “drains”; probably 2 from your neck and 1 from your donor site. You may have a saline drip for a while. If you’ve had a reconstruction, you may have a “Doppler” device attached to the flap to monitor blood flow.
Top tip – It’s a long operation and you’ll have had LOTS if anaesthetic and opiates. If you are prone to constipation ask for laxatives SOONER rather than later! Please!!
You may well not be able to swallow properly and I was given a long “wand” to suction out any build-up of mucus at the back of my throat. Coughing is clearly problematic, but you might be able to clear stuff by exhaling quickly. Over the next several days, gradually, drains start to get removed, dressings taken off, etc. etc. A trach I think normally stays in for 5-7 days.
Your neck and cheeks will be very swollen for quite some time – although yet again, everybody is different. The post-surgery swelling is “not” the same as swelling from lymphoedema but you will almost certainly be visited by a physio to assess your mobility and to give you exercises for neck, shoulders etc.
Depending on the surgery/healing/protocol, you’ll probably be given a “swallow test” under X-ray – though why they give you the gloopiest, most foul tasting stuff for your first swallow I don’t know! In theory I “failed” but my consultant saw me sip water the next morning and said I was good to go!
Discharge from hospital
You will be KNACKERED. Sleep and heal. Do not expect everything to go back to normal any time soon. It is MAJOR surgery. Be careful of your wound sites. Internal Infection is not uncommon either (however careful the surgeons, your mouth is an inherently dirty place). You will probably have been told to rinse frequently with salty water and probably have been prescribed Chlorohexidine mouthwash too.
Top tip – Any sign of redness, oozing, high temperature or quickened heartbeat, then get back in touch asap.
I found that my mouth was very dry initially but then I had periods of dribbling so much that I needed to stuff a tissue into the corner of my mouth!
Food – getting back to eating
Start gently – yoghurt, custard, purées. Tea is weird and very drying. Take it milky and/or weak. Coffee with loads of cream is much easier. Porridge may feel like eating gravel; try Ready Brek or very fine oats – maybe even put oats through a blender first. Very lightly scrambled eggs and tiny pieces of oily smoked salmon worked fairly early on. Puréed vegetables work well (though potatoes can be grainy); fish soup was my go to. Bread is evil and sticky.
Exercises, stretches and swallowing
You should continue exercises to maintain mobility to the best of your ability. Once you are swallowing reliably, you should also be given exercises to help maintain the strength of your swallow. This is especially important if you need to have Radiotherapy.
Follow-up with your consultant
Whether or not you will need any follow up treatment will depend on the histology of your tumour and lymph nodes. They will be sent to the lab and analysed for “margins” and other features on a cellular level. These results may take days or weeks and will be a decision for your Oncologist and the MDT (Multi-Disciplinary Team) which comprises surgeons, radiologists and oncologists.
Any follow up treatment you might need is likely to start between 6-8 weeks after surgery.
What next – am I cured?
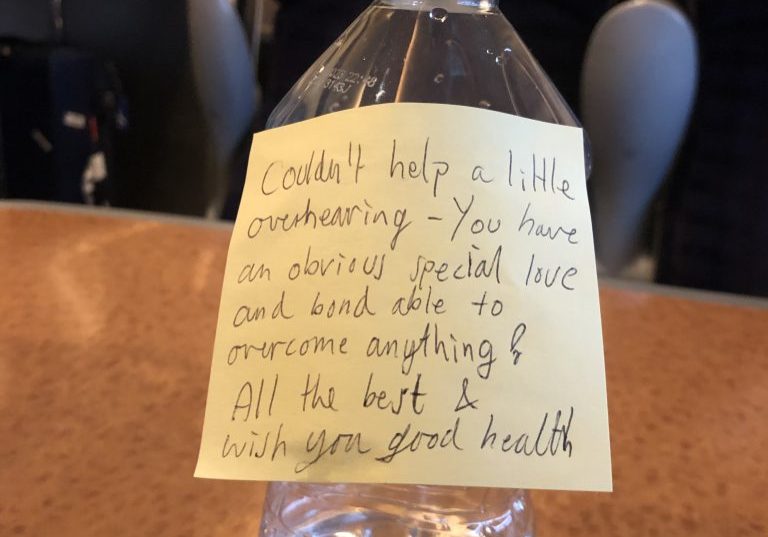
I had just been through the brutal surgery that has just saved your life, but what next? This is when I felt my most uncertain and my most fearful. My surgeon was overjoyed that my lymph nodes were clear and actually came to find me in X-Ray (my NG tube had moved?!).
My Multi-Disciplinary Team (MDT) had convened again to review my case and was split 50:50 post op – good margins, clear lymph nodes, but rubbish histology. Apparently the fact that’s I’d previously taken a drug called Methotrexate was known to probably make radiotherapy side effects worse!
It was “up to me”!!
I sought a second opinion from Professor Kevin Harrington at the Royal Marsden who had no doubts. So, essentially the decision was mine, but it was the “not really knowing” what to expect that scared me. I’d never forgive myself if I hadn’t done everything I could to prevent a recurrence. That angst was difficult enough to manage as it was!
So I decided that in order to “mop up” any cancer cells that may be around, I´d take the Radiotherapy. I was told that it would be 30 cycles (or doses) over 6 weeks but no chemotherapy.
Radiotherapy for tongue cancer, post surgery
Once you embark on radiotherapy treatment there are LOTS of acronyms, so I’ve tried to include most of those that you might meet. Radiotherapy to head and neck cancer is often, but not always, referred to “Adjuvant” treatment (added on) to a previous surgery. There is an overwhelming amount of information to absorb and is not really comparable to Radiotherapy to other parts of the body but it is still the standard recommended treatment.
Every Trust/Hospital seems to have a slightly different protocol but they should supply you with information and medication as well as making recommendations depending on your specific case. The Maxillofacial/Ear Nose and Throat (ENT) departments will convene an Multi-Disciplinary Team (MDT) meeting or a Tumour board, comprising Surgeons, Radiographers, Oncologists and nurses to review every individual case.

They will have looked at the results of any biopsies, histology (analysis of biopsies, and tumours) the size of the tumour and the depth of margins around it. They will look at the histology to see if there has been Peri-Neural Involvement (nerves), the way that the cancer cells are dividing (moderately/poorly differentiated cells) and the type of margin around the tumour (mine were “non-cohesive”).
If there has been spread to the lymph nodes in the neck, Radiotherapy will almost certainly be recommended. Many people will have chemotherapy too. Oral Squamous Cell Carcinoma (OSCC) is an aggressive cancer and even with good margins and no spread, Radiotherapy maybe recommended to “mop up” any stray cells which may be floating about.
Radiotherapy kills both good cells and cancer cells, but your DNA allows the good cells to regenerate, whereas the cancer cells can not.
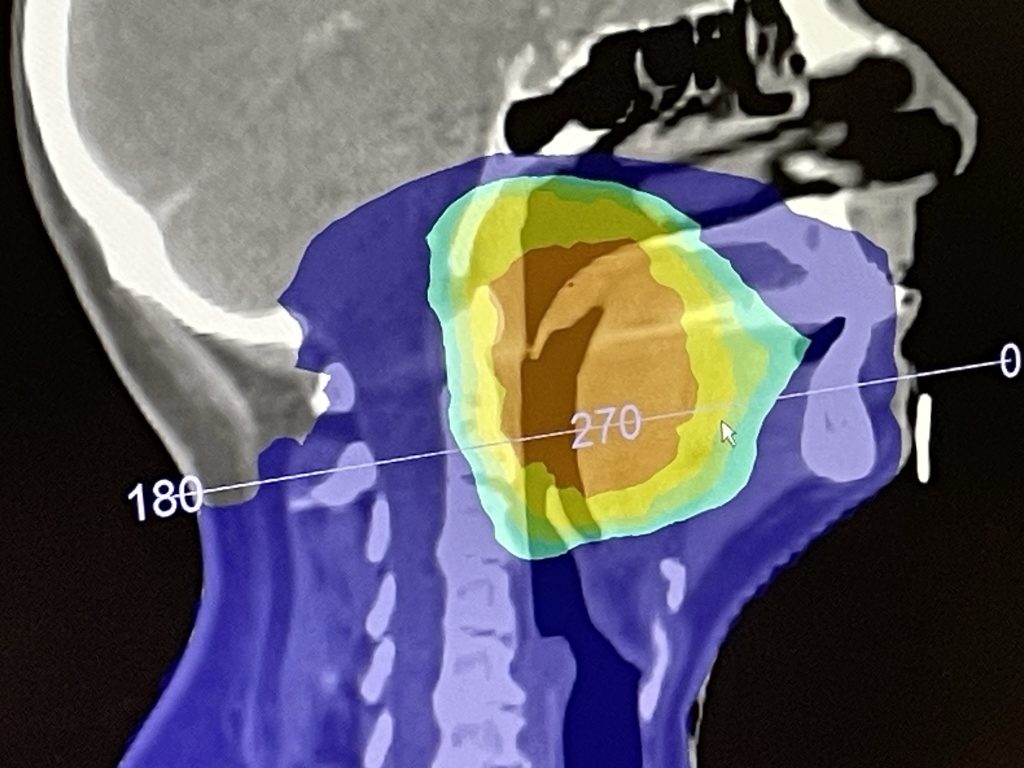
Radiotherapy Planning
The mask-fitting involves warm plastic being moulded to your head and neck. Some Cancer centres include a tongue depressor to ensure your tongue is always in the same place. I wasn’t able to tolerate this.
A CT scan is taken along with a mask-fitting and your Oncologist will make a plan especially for your particular case, deciding exactly where to target the Radiotherapy. The usual “dosage” is approximately 60Gy (Gray) over 30 – 35 sessions/“fractions” (6 – 7 weeks), but your oncologist will make recommendations for your particular case. There are also studies being made into shorter and more intense courses of treatment.
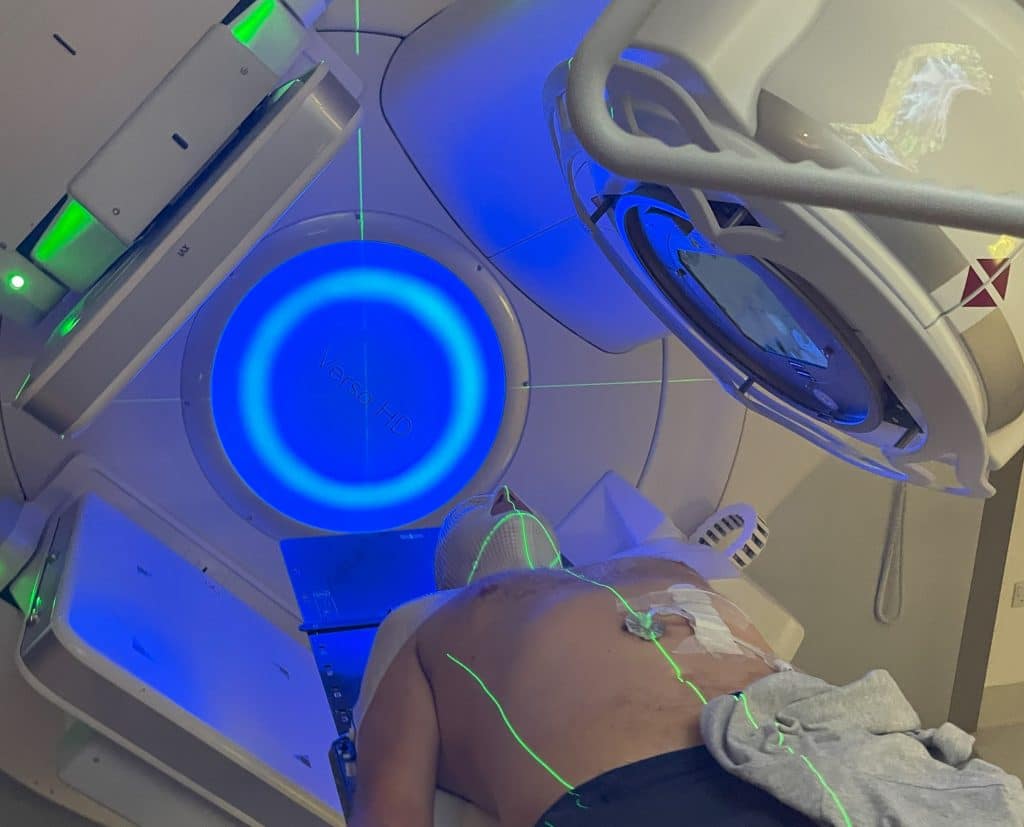
Most machines are “Linac machines” (Linear Accelerator) delivering Intensity-Modulated Radiation Therapy (IMRT). Proton Beam therapy is newer and is supposed to be more targeted, but there are few machines in the UK and results still seem to be inconclusive.
Preparation at home
Top tip – Eat NOW! You WILL lose weight. Get the protein in to aid healing.
Extra pillows are a good idea to prop you up in bed, resulting in less pressure from your teeth on your tender mouth and making it easier to nose-breathe (helping to avoid a dry mouth).
Prepare easy, soft food and soups in advance for the freezer
Consider buying a Humidifier to help with dry mouth symptoms. I quite liked adding essential oils and having an extra nightlight.
Radiotherapy Treatment
Top tip – DO ask for eye holes to be made. This allowed me to see the rest of the room and to watch the machine whirring & changing above me. You may be allowed nose holes too.
Your radiologists should do their best to make you feel comfortable by repositioning you in the mask or by adding “spacers” if you’re feeling too much pressure on your face. Lasers and a very quick scan check that you are in position. Final adjustments are made by moving the table itself.
You can not feel the “zapping” at all, but it can be unpleasant and uncomfortable to be bolted down to the table, especially if you develop blistering. Some centres play music; you may be allowed to bring your own, but the time is so short I thought that it barely seemed worth it. Some meditate, some listen; some need sedation. Whatever works for you.
The ideal window is to complete treatment is before 14 weeks/100 days. This is the “Package Time”. If you’ve had surgery, this should give a decent window for some recovery beforehand.
Wear comfortable clothes – no jewellery or metal. You may be offered a robe. I used to just pull down a soft bra and cover myself with a large scarf! Make sure you’re comfortable; it will make each session that much quicker for you and the Radiologists.
At the treatment centre
Top tips:
- Make sure you have Transport arranged. You may be able to drive to start with but maybe not towards the end of treatment.
- Take water with you and hydrate.
- Moisturisers and lip salve for AFTER treatment
- MAKE SURE YOU HAVE THE DIRECT LINE TO EMERGENCY CARE.
You will probably have a weekly appointment with your Oncologist. Write a list of questions as you go through the week and take it with you. No question, no concern or symptom is too trivial. Ask them all and don’t be rushed.
Dental matters
Before Radiotherapy, you should have a dental assessment to check that all your teeth are in a decent state & that it’s not likely that any will need to be removed in the near future. Some people may need extractions as a precautionary measure. Radiotherapy affects the small blood vessels and impairs the blood supply to the jaw. Socket healing following an extraction can therefore be problematic.
It is virtually impossible to avoid sugary foods during treatment if you want to maintain your weight, however Radiotherapy attacks the Parotid glands which produce saliva, reducing the quantity and altering its quality. As a result your teeth need to be given as much protection as possible.
Toothbrushes – Brushing can be difficult, but it’s really important. Oral-B make a sensitive, long head which is useful for an electric toothbrush. Baby toothbrushes may be better tolerated after the first few weeks of treatment. Warm water may help to soften bristles. When all else fails, then “lollipop stick” sponges are useful.
Toothpastes – Strong flavours – especially mint can be difficult during Radiotherapy.
- Oranurse is very gentle, non-foaming, no flavour with fluoride 1450ppm
- Oralieve & Biotene – toothpastes designed specifically for dry mouth with xylitol/sorbitol; fluoride- 1450ppm but they both have a minty flavour.
- High fluoride toothpaste – can be prescribed by your dentist or GP. You should be looking for fluoride 5,000ppm eg. Colgate Durophat but there are also various unbranded versions.
However, the mint taste of the high-fluroide pastes can be very difficult to tolerate during Radiotherapy. It might be worth using on interdental brushes if you’re able.
Mouthwashes for dry mouth & oral hygiene;
- Biotene
- Oralieve
- BioXtra – (my favourite) gentle mint and also contains fluoride 1500ppm
- Corsodyl/Chlorohexydine – useful after surgery to avoid infection and thrush, but it contains alcohol and you should avoid during Radiotherapy. Long-term use of Chlorohexydine can result in staining. I was told not to use it within 30 minutes of anything with fluoride.
- Tooth “Mousse” CM MI Paste plus a topical cream containing casein and fluoride for use last thing at night. ££ but I like the strawberry flavour! The “plus” version contains fluoride.
- Fluoride “trays” – seem to be recommended more in the US than elsewhere.
Radiotherapy side effects
Everyone is different and every NHS Trust seems to have a different protocol! Short-term side-effects:
- Lip blisters
- Gums go white
- Mouth blisters
- Throat blisters
- Exterior skin burning
- Muscle stiffness
- Increased puffiness in cheeks
- Increased lymphodoema
- Possible trismus
- “Flap” turns white
- Loss of taste
- Metallic/salty taste in your mouth
- Fatigue – ongoing. Solution – naps, extra sleep and good nutrition

First symptoms usually start to kick in at the end of week 2. Skin and lip care is super important. Use PH-neutral non-scented hair and skin products, e.g. Johnson’s baby shampoo, Dove soap and Simple products
No moisturiser before you have your radiotherapy. Apply lotions and potions AFTER treatment and not before, for eaxmple Aloe Vera gel, Aveeno cream and Aquaphor. There have been recent studies into the efficacy of chamomile gel
If your skin starts to burn, tell your team. Flamazine Ointment is highly recommended for helping burning skin to heal
Lip salves – Dr Bronners, Burtz Bees. Avoid anything with strong flavours. When my lips started blistering, sticking together and bleeding overnight, applying Gelclair mouthwash seemed to help (see below).
MUCOSITIS – inflammation/blistering of the mucosa (soft tissue inside mouth). This seems to be virtually unavoidable unless you are one of the lucky ones, but everybody has a different experience.
Mouthwashes – Keep the pH in your mouth nice and high (alkaline) – rinse constantly with a home-made solution of salt and bicarb throughout the day. It keeps your mouth clean, aids healing and helps prevent thrush. I was given Tellodont tablets (pink dental fizzy stuff) which does the same job and which I still use. Chamomile tea is also suppose to be soothing.
- “Healios” mouthwash seems to be advocated in a lot of US groups and “claims” to help prevent mucositis. Start a week before treatment. It’s glutamine based and is expensive – especially to send outside the US. Do check with your team first.
- “Raspberry mucilage and dispersible aspirin”: slightly old-fashioned local pain relief with a raspberry flavoured coating – to be used 10 mins before eating.
- Caphasol – not used by me, but some say good results for both prevention and treatment of mucositis.
- Gelclair; sachets of gel – diluted to provide pain relief and coating of the mucosa before eating. Can be used in combination with Raspberry Mucilage and aspirin.
- Difflam (benzydamine hydrochloride) is essentially a liquid anti-inflammatory used got pain relief. It can be diluted with water if too uncomfortable neat and also comes in spray form.
- Liquid Lidocaine – mouth numbing.
- Oxetacaine – pain-relief plus antacid
- “Magic mouthwash” – different “recipes” seem to be available in different countries! Most contain liquid/viscous lidocaine: some seem to include anti-histamines, steroids and anti-thrush medications as well as pain relief. Again, consult your team first.
- Mucosamin – given to me as a sample. Claims to help mucositis, but I found it far too minty during Radiotherapy. I now use it occasionally to almost moisturise my native tongue if it feels dry and rubbed.
Pain-relief during radiotherapy
Don’t suffer needlessly. It’s pointless being “brave”. If you’re in pain, do ask for additional pain-relief to allow you to eat. You need nutrition – especially protein – in order to heal. Pain medications should all be prescribed and monitored by your Cancer Centre. You may well prefer them in liquid or soluble form.
- Regular Paracetamol (surprisingly effective)
- Codeine
- Cocodamol (paracetamol plus Codeine)
- Oramorph (liquid short-acting morphine)
- MST (long acting morphine)
- Fentanyl (synthetic strong opioid, usually prescribed as patches & less constipating than morphine).
I was much happier once I had a long-acting drug which meant I didn’t have to top-up every 4 hours, which meant I could get some decent sleep. Think ahead and make sure you have adequate supplies – especially over the weekend. Make sure they don’t try and wean you off too quickly.
Top tip – Don’t forget the laxatives once you start opioids!!
MAKE SURE YOU HAVE THE EMERGENCY CONTACT NUMBER
Excessive thick Mucous
- Steam – shower, over a bowl or nebuliser machine.
- Diet, fizzy ginger-beer can help to cut through the mucus and possibly help with nausea too.
- Guaifenesin (Mucinex) can be prescribed. It’s also an ingredient in many over the counter cough medicines
Nausea
This is not something I experienced much of; but do mention it to your team and they will prescribe anti-nausea meds. Ondansetron is one good option, but can be constipating!
Dry mouth
This can be a long-term side-effect. If you are in the UK, contact The Swallows Charity who will provide a free box of sample products so you can find out what works best for you.
Most companies do a complete range. It’s a case of trial and error to see what works for you. Ingredients vary! Examples include; Biotene, Oralieve, BioXtra, AS Orthana, Saliveze
- Toothpaste – specially formulated for dry mouth with xylitol and fluoride
- Mouth Sprays
- Gels
- Mouthwashes (BioXtra mouthwash includes fluoride too 1,500 ppm)
In the UK, your GP should be able to write a prescription for all of these apart from the toothpastes. They WILL prescribe high-fluoride toothpaste 5,000 ppm
Xylimelts are useful overnight. A single lozenge with a slightly sticky surface is stuck to you gum which will dissolve slowly. They take a bit of getting used to initially.(not available on prescription).
Chewing-gum can be good once you have the confidence to chew. It also promotes jaw strength. Starbursts don’t contain mint flavourings. When all else fails, the drug pilocarpine can be prescribed. Some people find some success with Auricular Acupuncture, but results are not proven.
Exercises to avoid stiffness post-operatively & post-Radiotherapy
Your Cancer centre “should” provide you with a list of exercises. In the UK, it’s the Speech & Language Therapy Team (SALT) and they are also responsible for maintaining your “swallow”.
Physical Exercises – You will have been seen by a physiotherapist as soon as the day following any operation, however, these continue to be very important as Radiotherapy can increase any stiffness that you might experience. Work especially on keeping your neck and shoulders mobile. Keep practising jaw opening to avoid trismus. You can be prescribed a “Therabite” machine to help maintain jaw mobility.
Top tip – keep swallowing – exercises to re-educate muscles are an important part of your long-term rehabilitation
Lymphoedema – If your lymph nodes are removed in a neck dissection, then your lymph has no route to travel through your body. Until it develops a new route lymphoedema (swelling) can develop which can be unsightly and at its worst can become infected. You can ask for a Clinic referral.
Self-massage – There are several YouTube channels, this is one of the best I have found:
https://youtube.com/c/CancerRehabPT
Nutrition – You should be given a consultation with a dietician before, during & after treatment. Food supplements/shakes should be prescribed as required to maintain your weight – both for your health and to make sure that your mask continues to fit. The first 10-14 days should be tolerable, after which eating can start to get difficult and will continue to be so for several weeks after treatment ends. Again, everyone is different and very often it’s 2 steps forward and 1.9 steps backwards again.
Top tip – I ate in a restaurant 6 months after treatment, so don’t lose hope!
Food & recipes are covered here, but – try to keep up your protein intake. Prepare stuff for the freezer beforehand. Vitamins and supplements are not recommended during Radiotherapy.
Foods that worked for me in the early months after treatment
Breakfast
Greek yoghurt plus puréed tinned fruit – peaches and pears
Coffee and cream
Lunch
Scrambled eggs with added Philadelphia/cream cheese
Smoked salmon – nice and oily
Gently fried eggs
Brioche – and lots of butter
Croissants – and lots of butter
Pâté
Quiche – 30 seconds in the microwave
Supper
Soups plus cream – seems to make them lighter.
Poached fish – 5 minutes in milk/water
Fish, rather than chicken;
Chicken leg rather than chicken breast;
Rare meats, rather than well-cooked (once you’re no longer too vulnerable to infections etc).
Sweet potato rather than potato (gets very grainy and sticky when mashed)
Fresh Ravioli
If you’re desperate for salad, try chopping finely and mix with Cottage Cheese.
Chocolate mousse
Cream doughnuts!

Foods to treat with caution
Taste/chemicals – tomatoes & vinegar; acidic fruits, black pepper and chilli´s; onions, garlic and leeks
Texture can be difficult – either irritating or excessively gloopy.
Supplements drinks – These should be provided by your dietitian/SALT team or GP
Pre-mixed eg. Ensure (I found “2cal” far too thick and gloopy – nauseating – and moved down to Ensure Plus). Fortisips multiple flavours.
Powders – add water or milk; various brands and flavours – vegetarian, vegan etc. At one stage only vanilla was tolerable.
Some find it helpful to cool them in the fridge beforehand or to thin them out with water or milk.
Tube feeding
Covered here, but if you are not getting adequate nutrition, then do not discount these options; NG (naso-gastric) tube, PEG and RIG.
If you´ve been affected by Stessy´s story
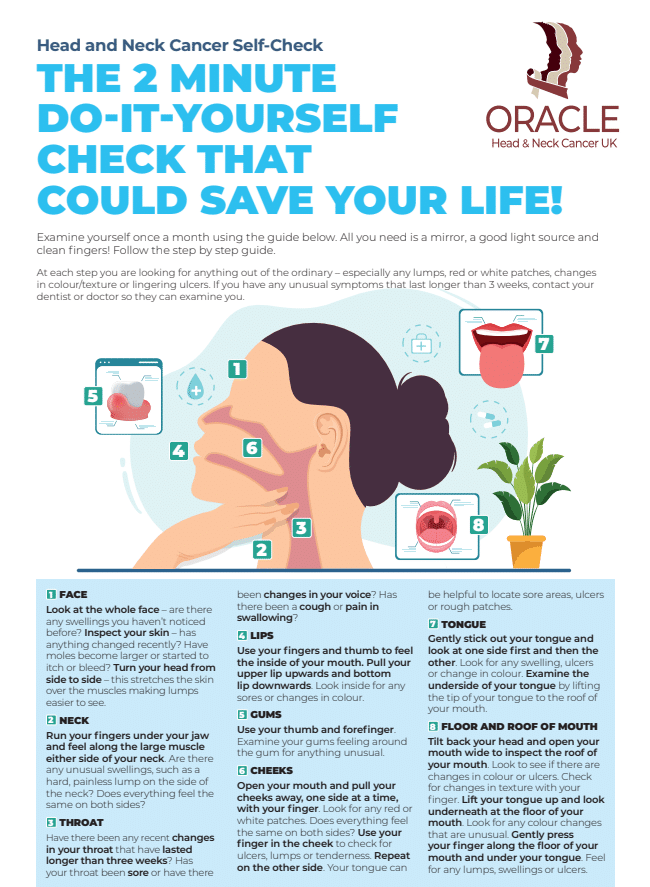
Let’s all take action to prioritize our health and raise awareness for early detection.
If you´re worried about changes in your voice, neck or mouth please refer to our simple “home check” guide.
See also other patient stories to hear about other people diagnosed with Head and Neck Cancers.
Have you got a symptom, are you being diagnosed, going through treatment, or a friend/carer of someone who is?
Please join our private Facebook Group to get support and advice from fellow patients and carers.
#headneckcheck
Regular self-checks play a vital role in the early detection of Head and Neck cancer
Patient Stories

Suzie Cooke – a lesson in not taking ‘no’ for an answer

Nigel Lloyd-Jones – being told “you have cancer” is life changing

Belinda Gilfoyle – a slow recovery and learning to stay positive

Salivary Ductal Adenocarcinoma news “hit me like a train”